Dr. Mamadu Baldeh is a 31-year-old medical officer attached to the Infectious Disease and Isolation Unit at the Connaught Hospital, University of Sierra Leone Teaching Hospital complex, in Freetown, Sierra Leone.
news
Sept. 19, 2020
AFRICA RENEWAL
4 min read
We have a responsibility to invest in our healthcare system: Dr. Mamadu Baldeh

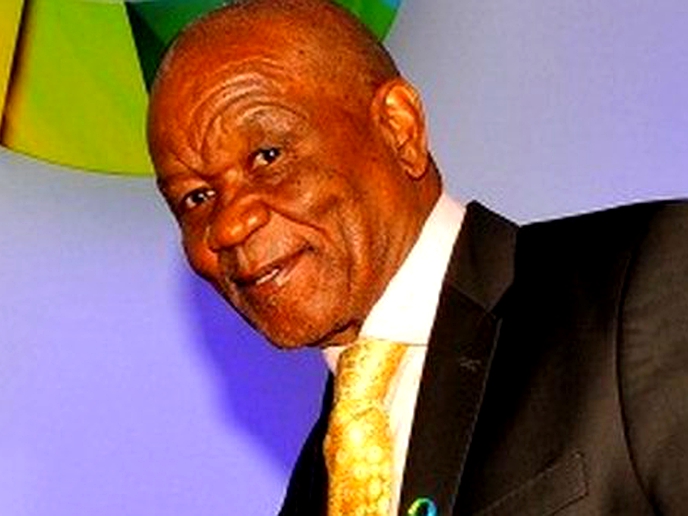
Dr. Mamadu Baldeh, a medical officer attached to the Infectious Disease and Isolation Unit at the Connaught Hospital
Can you tell us a bit about yourself?
I am Dr. Mamadu Baldeh, a 31-year-old medical officer attached to the Infectious Disease and Isolation Unit at the Connaught Hospital, University of Sierra Leone Teaching Hospital complex, in Freetown, Sierra Leone.
I am also a clinical research assistant and anatomy demonstrator at the College of Medicine and Allied Health Sciences, University of Sierra Leone. I am the president of the Junior Doctors Association of Sierra Leone.
How long have you been working as a healthcare worker? What made you choose a career in healthcare? Any fears or regrets?
I have been a medical doctor for almost four years, providing clinical care to patients as well as teaching medical students at the University of Sierra Leone. My first clinical experience after leaving the medical school was serving as a volunteer medic during the 2016 Olympic Games in Río de Janeiro, Brazil.
I grew up as a scout, so service to others brings me satisfaction. As a child I envisaged a career of service: taking care of people in pain and discomfort. I therefore decided to become a doctor.
My biggest fear is when patients die because of lack medical facilities. We have amazing medical practitioners in Sierra Leone, but we need to be empowered.
How are you helping fight COVID-19 in your country? How has your work changed since COVID-19 broke out?
As the officer in charge of the largest isolation unit for COVID-19 in Sierra Leone, I see patients who are sometimes in critical state. We provide each suspected case with a set of bedside vital equipment, rapid diagnostics test and emergency medications. These will help reduce possible risk of cross-transmission infection.
Most cases nationwide pass through our facility. As the only doctor attached to the unit, I sometimes sleep at the facility attending to patients.
What affects you the most in this COVID-19 situation? What keeps you going? How are you coping?
What affects me include explaining to patients with mild symptoms that they are positive for COVID-19. Sometimes, a patient may question a lab result or even our medical judgment. But we keep motivating ourselves within the unit to do the best we can for all our patients.
Also, most cases that come to our unit are highly suspected for COVID-19 but may include long-standing co-morbidities. Therefore, after testing, irrespective of whether it turns out to be COVID-19 or not, there is some unfavorable news for a patient with underlying conditions.
Finally, with no active general testing programme to identify asymptomatic or mildly symptomatic patients, those who eventually get tested are likely to be already showing severe symptoms of COVID-19, which complicates management of the disease.
Enjoy our daily newsletter from today
Access exclusive newsletters, along with previews of new media releases.
Considering that a huge percentage of the population live on daily earnings, available resources should be diverted to supporting families during an extensive lockdown such as two to three weeks or more.
What strategy, in your view, has worked well in this fight and what has not? What should be done to win the war against COVID-19?
In the early days of the fight against COVID-19, it seemed we were ahead of the virus. We were among the last countries in the world to register a case. Measures like community sensitization, messages of hygiene etiquette, social distancing and closure of the international airport were all actions that yielded good results.
Considering that a huge percentage of the population live on daily earnings, available resources should be diverted to supporting families during an extensive lockdown such as two to three weeks or more. Lockdowns disrupt the incubation period of the virus and greatly reduce community transmission. They also give us enough time to screen, assess suspected communities and to isolate asymptomatic patients.
Second, we need to procure more test kits and perform more tests. Healthcare workers need (personal protective equipment) PPEs to keep fighting the virus.
Face masks should be obligatory for everyone outside their homes.
Finally, information to the public must be consistent. To counter fake news, we should not have discrepancies in the information we communicate to the general population.
What is your message to people in your country and to fellow Africans in general, at this time of COVID-19?
My message is that COVID-19 is real, and the best shot we have to win the battle is by following measures put in place by authorities, including the use of face masks, observing social distancing, regular handwashing and other hygiene etiquettes. These measures will help flatten the curve.
My message to authorities is, please enhance our testing capacity.
We have a responsibility to invest in our healthcare system always, and not just during a health crisis.
For more information on COVID-19, visit www.un.org/coronavirus
Tailored for you